Colorectal cancer models overview
Colorectal models:
Colorectal-specific tools
Background
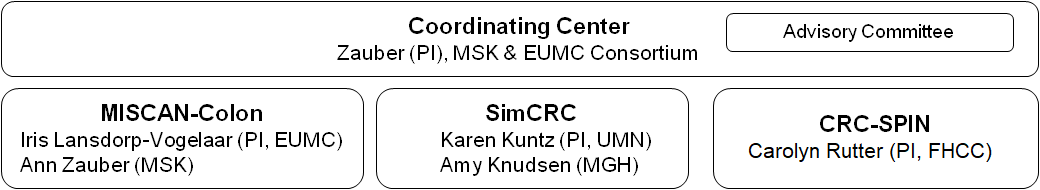
The CISNET-CRC group is composed of three independently developed state-of-the-art colorectal cancer (CRC) microsimulation models for the evaluation of interventions, with emphasis on screening. The three models and their corresponding sites are: 1) MISCAN-CRC with investigators from Erasmus University Medical Center (EUMC) and Memorial Sloan Kettering Cancer Center (MSK); 2) SimCRC from the University of Minnesota (UMN) and Massachusetts General Hospital (MGH); and 3) CRC-SPIN from Fred Hutchinson Cancer Center (FHCC) (Figure 1). All models describe the natural history of CRC using different underlying structures, reflecting different philosophies across groups. These differences allow model comparisons to explore the impact of structural uncertainty. Our ultimate goal is to reduce the impact of CRC by providing the information needed to address key policy questions and prioritize future CRC research. We aim to achieve this goal by using the models to simulate a population(s) in order to evaluate the impact of colorectal cancer screening.
MISCAN-Colon: MIcrosimulation SCreening Analysis (MISCAN) Colorectal Cancer Model
SimCRC: Simulation Model of Colorectal Cancer
CRC-SPIN: Colorectal Cancer Simulated Population model for Incidence and Natural history
Figure 1 Organization of the CISNET-CRC Group
Recent Studies
Questions surrounding the comparative- and cost-effectiveness of colorectal screening tests led to the development of the three colon microsimulation models. Soon after, the United States Preventive Services Task Force (USPSTF) commissioned the Colorectal Group models to guide their recommendations for optimal screening strategies, most effective ages to begin and end screening, and intervals for screening with stool-based tests (e.g., Fecal Occult Blood Test, Fecal Immunochemical Test, stool DNA) and direct visualization tests (e.g., sigmoidoscopy, colonoscopy, CT-colonography).1,2 In addition to the USPSTF recommendations, the models have been used for local area screening3, examining the U.S. public health impact of achieving 80% CRC screening4, estimating future colonoscopy need based on current volume and capacity to screen5, and ongoing studies looking at screening recommendations for genetically predisposed patients such as those with Lynch Syndrome or Cystic Fibrosis.
Overall Model Structure
All three colorectal models are stochastic microsimulation models. The term "stochastic" implies that the models simulate sequences of events by drawing from distributions of probabilities or durations randomly rather than using fixed values. The term "microsimulation" implies that persons are moved through the model one at a time (individually) rather than as proportions of a cohort. This allows future state transitions to depend on past transitions, giving the models a "memory". Further, unlike most traditional Markov models, the models do not use yearly transition probabilities; instead, they generate durations in adenoma and cancer states, thereby increasing model flexibility and computational performance.
Simulated individuals in the model reflect the natural history of colorectal cancer (CRC) using a structure that builds upon the adenoma-carcinoma sequence.6,7 Persons begin disease free (i.e., no lesions) and, with the absence of a screening intervention, can move through several disease states by developing one or more adenomas. The adenomas can grow in size, possibly develop into cancer (e.g., adenoma, preclinical, clinical stages I to IV), and death from CRC or from competing risks can occur at any time. Survival after clinical diagnosis is determined by the stage at diagnosis, the localization of the cancer, and the person's age.
Time Scale
All models describe events in continuous time.
Adenoma Risk
All models allow for development of multiple adenomas. Adenoma risk varies stochastically across individuals and by age (≥20 years), although the models use different underlying mechanisms to generate the adenoma natural history. All models have or can generate specific distributions for the location of adenomas in the colorectum based on data from autopsy studies (SimCRC and CRC-SPIN) or the distribution of clinically detected CRCs shown in Table 1 (MISCAN-CRC). Adenoma growth in all models varies randomly across individuals, and across adenomas within individuals, with size categories as small (≤5 mm), medium (6-9 mm), and large (10+ mm) (MISCAN-CRC and SimCRC) or continuously with a minimum size of 1 mm and maximum size of 50 mm (CRC-SPIN).
Progression to (Pre)clinical Colorectal Cancer
The progression to preclinical and clinical CRC in all models is dependent on adenoma size (generally > 6mm) and independent of adenoma progression rate within individuals. In the MISCAN-CRC and CRC-SPIN models, the probability that an adenoma progresses to preclinical cancer depends on age at adenoma initiation. In the SimCRC and CRC-SPIN models, adenoma progression depends on location in the colorectum. All models allow multiple preclinical cancers and assume that when one preclinical cancer is detected, all preclinical cancers are detected. Data on clinical progression are derived from the Surveillance, Epidemiology, and End Results (SEER) program incidence rates.
Risk Factor Modeling
Both the MISCAN-CRC and SimCRC models can include risk factors, and their basic models can describe CRC by race. CRC-SPIN has a general risk factor model, but it is not calibrated and does not currently include specific risk factors.
MISCAN-CRC and SimCRC include the same set of eight risk factors (obesity, smoking, red meat consumption, physical activity, fruit and vegetable consumption, multivitamin use, aspirin use, and hormone replacement therapy). MISCAN-CRC includes all risk factors using binary indicators and only allows risk factors to influence adenoma onset. SimCRC uses a mix of dichotomous and continuous risk factors, and they may affect both adenoma onset and adenoma progression. Both MISCAN-CRC and SimCRC use the SimCRC module to describe risk factor prevalence, which accounts for correlation among the risk factors using NHANES data. The SimCRC risk factor module was calibrated using data from the National Health Interview Survey (NHIS) and Health Professionals Follow-Up Study (HPFS). MISCAN-CRC used published relative risks from the same datasets to estimate the effect of risk factors on adenoma onset.
Death
All three models stochastically assign CRC death using survival probabilities based on Cox proportional hazards models for relative survival applied to Surveillance, Epidemiology, and End Results (SEER) survival data for cases diagnosed from 1/1/1975 to 12/31/2003 with follow-up through 12/31/2010.8 Time to CRC death depends on stage, location (colon or rectum), age at diagnosis, year of diagnosis, sex, and (optionally) race. The SimCRC model also has a separate post-CRC-diagnosis model that simulates the risk of subsequent metastatic recurrence and only allows CRC deaths to occur following an unresectable metastatic recurrence.
All models also stochastically assign non-CRC death using life-tables from the National Center for Health Statistics. In addition, Dr. Wang, as part of SimCRC's collaborative CISNET work, developed life table adjustments that allow the models to incorporate the effects of obesity and smoking behavior on the risks of non-CRC death.9 Similarly, Dr. Cho developed life table adjustments that allow incorporation of the effects of comorbid conditions on non-CRC death.10
Screening
Differing colorectal cancer screening intervention modalities are evaluated by the models. There are two types of screening tests used for colorectal cancer: stool-based tests and direct visualization tests. Stool-based tests include guaiac fecal occult blood test and fecal immunochemical test (with and without DNA sampling), and direct visualization tests include colonoscopy, sigmoidoscopy, and CT colonography. All models apply screening test sensitivity and specificity rates from existing literature and/or reports from the company/manufacturer. Sensitivity analyses are performed based on the best and worst case screening scenarios, which include the lowest and highest test sensitivity/specificity rate reported. Doing so provides estimates of possible screening effects for the population of interest.
Table 1. Distribution of Adenomas in the Colorectum, by Model, averages across ages 40-100 years
| Location | MISCAN-CRC | SimCRC | CRC-SPIN |
| Cecum | 0.16 | 0.10 | 0.08 |
| Ascending colon | 0.08 | 0.23 | 0.23 |
| Transverse colon | 0.12 | 0.29 | 0.24 |
| Descending colon | 0.06 | 0.09 | 0.12 |
| Sigmoid colon | 0.36 | 0.21 | 0.24 |
| Rectum | 0.21 | 0.08 | 0.09 |
MISCAN assumes that the distribution of locations of adenomas across the colon and rectum has the same distribution as the locations for CRC. The distribution of location of adenomas in the SimCRC and CRC-SPIN models is based on the distribution of location of adenomas observed in autopsy and/or colonoscopy studies.
References
- Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Annals of internal medicine. 2008;149(9):659-69.
- Knudsen AB, Zauber AG, Rutter CM, Naber SK, Doria-Rose VP, Pabiniak C, et al. Estimation of Benefits, Burden, and Harms of Colorectal Cancer Screening Strategies: Modeling Study for the US Preventive Services Task Force. Jama. 2016;315(23):2595-609.
- van der Steen A, Knudsen AB, van Hees F, Walter GP, Berger FG, Daguise VG, et al. Optimal colorectal cancer screening in states' low-income, uninsured populations-the case of South Carolina. Health Serv Res. 2015;50(3):768-89.
- Meester RG, Doubeni CA, Zauber AG, Goede SL, Levin TR, Corley DA, et al. Public health impact of achieving 80% colorectal cancer screening rates in the United States by 2018. Cancer. 2015;121(13):2281-5.
- Joseph DA, Meester RG, Zauber AG, Manninen DL, Winges L, Dong FB, et al. Colorectal cancer screening: Estimated future colonoscopy need and current volume and capacity. Cancer. 2016;122(16):2479-86.
- Morson BC. Evolution of cancer of the colon and rectum. Cancer. 1974;34(3):suppl:845-9.
- Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer. 1975;36(6):2251-70.
- Rutter CM, Johnson EA, Feuer EJ, Knudsen AB, Kuntz KM, Schrag D. Secular trends in colon and rectal cancer relative survival. Journal of the National Cancer Institute. 2013;105(23):1806-13.
- Wang YC, Graubard BI, Rosenberg MA, Kuntz KM, Zauber AG, Kahle L, et al. Derivation of background mortality by smoking and obesity in cancer simulation models. Medical decision making: an international journal of the Society for Medical Decision Making. 2013;33(2):176-97.
- Cho H, Klabunde CN, Yabroff K, et al. Comorbidity-adjusted life expectancy: A new tool to inform recommendations for optimal screening strategies. Annals of internal medicine. 2013;159(10):667-76.
